What is depression?
See your GP if you have feelings of depression
It’s important to see your GP if you think you might be depressed. Don’t delay getting help. The sooner you see your GP, the sooner you can get support and advice to help you recover and feel better.
Anyone can experience depression, and there are lots of different reasons why people might be depressed.
There are lots of organisations offering support and advice for various mental health conditions, including depression.
You may be depressed if you:
- have a low mood that lasts a long time (weeks or months) and affects your everyday life
- lose interest and pleasure in things you used to enjoy
- feel like you don’t have any energy.
If depression is mild, it may not stop you leading your normal life, but it can make everything feel harder to do and seem less worthwhile.
At its most severe, depression can make some people have suicidal thoughts.
Call 999 or go straight to A&E if:
you’re having thoughts about harming yourself or taking your own life
The NHS has more information and advice, including the symptoms to look out for.
Depression and your lung condition
Living with a long-term condition can be challenging. In fact, studies show that you’re two to three times more likely to get depression if you’re living with a long-term physical health condition, compared to someone who is in good physical health.
- If you already have depression, having a long-term lung condition could make your depression worse, especially if your condition limits what you can do on a daily basis.
- Also, the side effects from some medicines can increase the risk of becoming depressed, or make it harder to recover from depression.
- Living with a lung condition can sometimes cause problems in other areas of life too, like at work or school, if you need to take time off because of symptoms being worse.
- If your lung condition means you’re unable to do certain things, being depressed can mean you feel even less able to do things. This in turn can make you feel more depressed.
However, depression is less likely if your condition is well controlled.
You may find that with good support and treatment to help you deal with your depression, you’ll be able to manage your lung condition better and lower your risk of asthma attacks or flare ups.
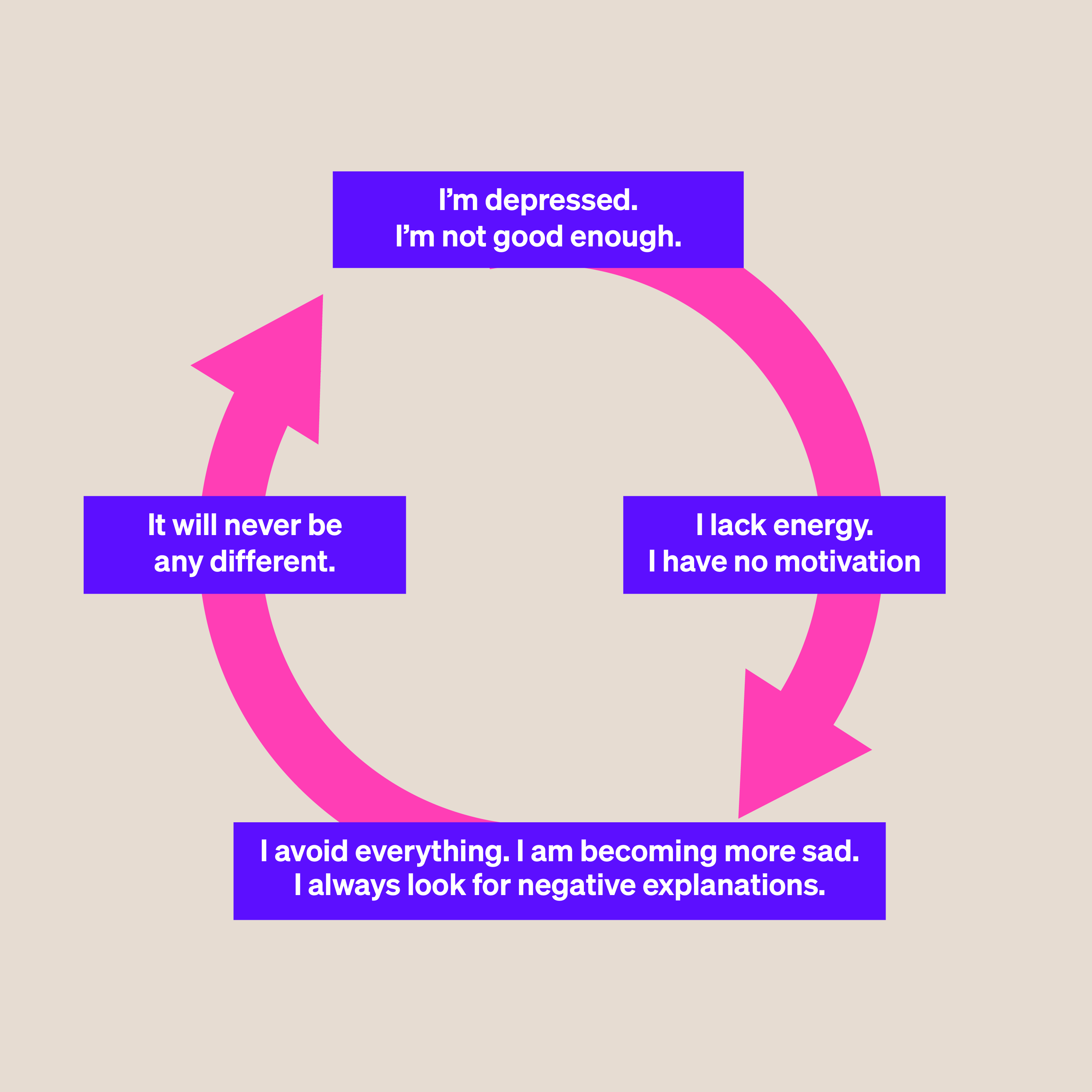
Break the cycle of depression and symptoms
Depression may make it feel harder to look after your lung condition properly. Then as your symptoms get worse, you may feel more depressed, and find it harder to get on top of your mood.
Try to break this cycle with three easy steps:
- Talk to your GP or specialist about all your symptoms.
- Do one thing today to help lift your mood. For example, you could call a friend, go for a walk, or do something you enjoy doing but haven’t done for a while. Get more ideas from the NHS.
- Share your feelings with other people who have long-term lung conditions by joining our HealthUnlocked community. It could make you feel less alone.
Is depression a side effect of your medicines?
Talk to your GP, pharmacist, or other healthcare professional as soon as possible if you’re experiencing any side effects from your lung medicines.
They may be able to adjust the dose or support you in managing the side effects.
Not all medicines have depression as a side effect. But if you need to take high dose steroids for your asthma or lung condition, there is a higher risk of side effects, including depression.
Montelukast side effects warning
Montelukast is a leukotriene receptor antagonist (LTRA). It’s been linked to side effects like depression and anxiety. But these are not common, affecting between 1 in 100 to 1 in 1000 people. If you notice any changes in your mood, or your child’s mood, see your specialist, GP or nurse as soon as possible.
There is also a very rare possible side effect of suicidal thinking, that affects fewer than 1 in 10,000 people. If you do get this side effect, stop taking the medicine immediately and talk to your specialist, GP or nurse as soon as possible.
Treatments for depression
Your GP can talk to you about talking therapies and whether you’d benefit from some medicines for your depression.
It’s important to see your GP so you can get the right diagnosis, and the right treatments, for the kind of depression you have.
GPs will use different approaches depending on whether your depression is diagnosed as mild, moderate or severe.
There are lots of different treatment options for depression.
- talking therapies like cognitive behavioural therapy (CBT)
- support groups
- exercise therapy
- antidepressant medicines.
Your GP or specialist may also refer you to pulmonary rehabilitation (PR) or another group exercise class. Research has shown PR improves not only your fitness, but your mental well-being as well.
Your GP or healthcare professional can also give you advice if you’re thinking of complementary therapies like massage or meditation to help with symptoms of depression.
What is Cognitive Behavioural Therapy (CBT)?
CBT encourages you to think about your problems and find ways to deal with them. It looks at your thoughts and what you are doing (your behaviour) to identify negative cycles that may have developed.
This helps you to identify unhelpful thinking patterns or behaviour and develop ways to manage the difficulties you may be experiencing.
You can read more about CBT on the NHS website.
Taking antidepressants
Antidepressants prescribed by your doctor have been shown to work best when taken alongside counselling or other kinds of talking therapy such as CBT.
Antidepressants can relieve the symptoms of depression, while talking therapies can help you with the causes of your depression over the longer term.
Talking therapies also support you to manage your emotional well-being in the future.
There are lots of different antidepressants licensed for use in the UK.
Whenever you're starting to take a new medicine, you should always talk to your GP or a pharmacist about any medicines you're already taking. This is because there might be some antidepressants you need to avoid. For example, the anti-depressant fluvoxamine is not recommended for someone taking the asthma medicine theophylline.
Your healthcare professional can tell you which antidepressant is likely to work best for you.
They can:
- consider your lung condition and the medicines you take to manage it
- tell you about the possible side effects the drugs may have
- explain all the risks and benefits of particular types of antidepressants
There's no evidence yet that one particular anti-depressant is best for someone with a lung condition.
What about complementary treatments for depression?
Always speak to your GP or other healthcare professional before trying herbal treatments available without prescription from chemists or health food shops.
For example, St John’s Wort is not recommended by National Institute of Clinical Excellence (NICE). This is because it could react badly with other drugs, and because doses and strengths of the different products sold can vary.

Get support
Call our Helpline for support with your condition. Get advice on your medicines, symptoms or travelling with a lung condition, or just call us to say hello.




