What is peak flow?
Peak flow is a measure of how quickly you can blow air out of your lungs. If you have asthma, you may sometimes have narrow airways. This will make it more difficult to blow the air out of your lungs quickly and can change your peak flow score.
You measure peak flow by taking a full breath in and blowing out as hard and fast as you can into a small hand-held device called a peak flow meter.
Your peak flow score is also called your peak expiratory flow (PEF).

When is peak flow used?
Peak flow is mainly used to help diagnose and monitor asthma.
Peak flow to help diagnose asthma
You may be asked to keep a peak flow diary for two or more weeks to help your GP make an asthma diagnosis . This can show a pattern of peak flow scores over time that are not normal.
Alongside a clinical history, and other tests like spirometry and FeNO, peak flow can suggest you have asthma.
Peak flow to monitor asthma
Your GP or asthma nurse may do a peak flow test at your annual asthma review.
They might also ask you to check your peak flow at home. This means taking your peak flow every day and writing down your scores in a peak flow diary.
Doing this helps to see if your peak flow changes over time. It can help you understand when your symptoms are getting worse and what could be triggering them.
Monitoring peak flow could cut your risk of an asthma attack.
Checking your peak flow at home is most useful if you’re recovering from an asthma attack, or your treatment plan has changed.
Talk to your GP or asthma nurse about whether you need to monitor your peak flow, how often and what to do when your scores change.
See your GP if you’re getting symptoms
If you are having symptoms or need to use your reliever inhaler three or more times a week, see your GP, even if your peak flow scores are normal.
This is a sign that your asthma is getting worse.
How to use a peak flow meter
When you first get a peak flow meter, ask your GP, asthma nurse or pharmacist to show you how to use it and how to take a reading.
Take these steps to make sure you use your peak flow meter correctly:
- Pull the counter (the red arrow) back as far as it will go to the top near the mouthpiece.
- Stand or sit upright – choose what’s most comfortable for you, and always do it that way.
- Take the deepest breath you can.
- Make sure your mouth makes a tight seal around the mouthpiece.
- Blow as hard and fast as you possibly can into the meter.
- Write down your score (the number next to the pointer).
- Do this three times in a row, with a short rest in between, so you get three scores (all three scores should be roughly the same).
- Use the highest of these scores to fill in your peak flow diary.

How to use a peak flow meter
Hi I'm Naomi. I'm a respiratory nurse specialist at Asthma + Lung UK. I'm going to tell you how to use a peak flow meter.
When you first get a peak flow meter, ask your GP, asthma nurse or pharmacist to show you how to use it and how to take a reading.
If you're checking your peak flow at home, you need to take your peak flow at least twice a day, every day to get a useful pattern of results. Try to check it at the same time every morning and every evening.
You need to use your best effort every time you blow into the meter so you're comparing like with like and you should use the same peak flow meter every time.
Take these steps to make sure you use your peak flow meter correctly.
Pull the counter, the red arrow, back as far as it will go, to the top, near the mouthpiece.
Stand or sit upright. Choose what's most comfortable for you and always do it that way.
Then take the deepest breath you can and make sure your mouth makes a tight seal around the mouthpiece.
Then blow as hard and as fast as you possibly can into the meter, like this.
Write down your score which is the number next to the pointer.
Do this three times in a row with a short rest in between so that you get three scores.
All three readings should be roughly the same but don't worry too much if they vary. Use the highest of these scores to fill in your peak flow diary.
If you have any questions about using your peak flow meter speak to your doctor, nurse or pharmacist. You can also call our helpline.
If you want to monitor on your asthma using peak flow, you’ll get the most useful results if you:
- Check your peak flow at least twice a day, every day to get a useful pattern of results. Ask your GP or asthma nurse how often and for how long they would like you to take your peak flow readings.
- Check it at the same time every morning and every evening Remember, the earlier you do your peak flow test after waking up, the lower the score will be. This is because scores are naturally lower early in the morning.
- Use your peak flow meter before you take your asthma medicine or medicine for other lung conditions, otherwise it will change the score.
- Use your best effort every time you blow into the meter so you’re comparing like with like.
- Use the same peak flow meter every time.
- Write down your symptoms and what you’ve been doing too. For example, ‘I exercised on Tuesday’ or ‘I came into contact with a pet.’ There’s space for you to do this in your peak flow diary. This helps you and your GP or asthma nurse understand how different triggers affect your asthma and may help you prevent future dips.
- Take your peak flow diary to your asthma review and any other asthma appointments to show your GP, asthma nurse or consultant how your asthma has been.
- Always use an asthma action plan alongside your peak flow diary, so you know what to do if asthma symptoms get worse. There’s space on the plan for you to write down actions you and your GP have agreed if your peak flow score is lower than usual.
- Speak to your GP or asthma nurse or pharmacist If you’re finding it difficult taking your peak flow, or if you feel breathless or tight-chested afterwards.
- Clean your peak flow meter by washing it in warm soapy water, rinsing it with clean water, and leaving it to air dry.
Understanding your peak flow scores
Peak flow scores to help diagnose asthma
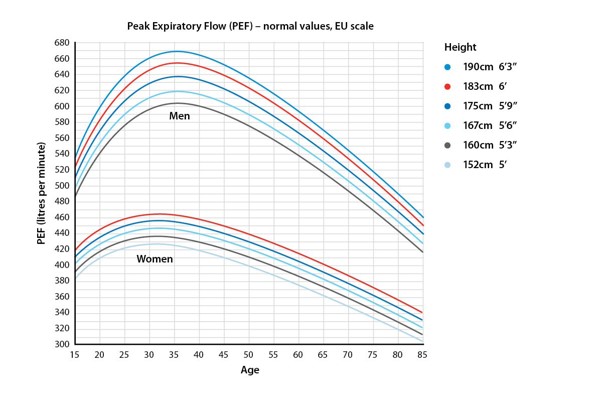
To help diagnose asthma, your GP can compare the peak flow score you get to the score usually expected for your age, height, and sex.
Your GP or asthma nurse will be looking for a pattern of scores that show changes which are not normal. If there’s a big difference between your score and a normal score, or when you have symptoms or not, it could suggest you have asthma.
Peak flow can vary at different times of the day too. For example, it’s normal for people to have a lower score in the morning. But if there’s a big difference between the scores you get in the morning or evening, it could suggest you have asthma.
Peak flow readings when you’re having symptoms that could be asthma can also be useful.
Peak flow scores to help monitor your asthma
How much your scores vary is important when you’re monitoring your asthma at home too.
The main thing is knowing the score that’s normal for you, or your best score. Then you can see if your score has dropped lower than your normal score.
See your GP or asthma nurse if your peak flow is much lower than normal
A big drop in your peak flow score could be a sign that your airways are tight and inflamed or that your asthma is getting worse.
Keep a peak flow diary
To understand your own peak flow, you need to see a pattern of scores over time. So, whether you’re using peak flow all the time, or you have been asked by your GP or asthma nurse to use it for two or more weeks, it’s important to note down your scores every day.
You can do this using a peak flow diary. Or you might want to use the calendar on your phone to note your scores.
You and your GP or asthma nurse can then look at the scores you’ve been getting and work out what score to expect when you’re well.
Your best score
The score that’s usual for you when you’re well is sometimes called your ‘best score.’
If you’re using your medicines as prescribed and following your asthma action plan, you should stay close to your personal best score most of the time.
If you’ve had a change of medicines recently, a good peak flow score can tell you that they’re working well.
You need to record your peak flow for at least two weeks to get a personal best score. Ask your GP to check your best score again if it’s been a few years since it was checked.
Lower than your best score
If you get a peak flow score that’s lower than your best score, this may be a sign of an asthma attack.
Getting a lower peak flow score can also help you find out if triggers , infections , or allergies could be making your asthma worse.
For example, you might notice lower peak flow readings when pollen’s high, you’ve got a cold, or when you’re at work.
In your peak flow diary, there’s a space to make a note if you’ve had symptoms or if there’s a reason why your readings could be lower than normal.
Talk to your GP or asthma nurse about what low scores you need to look out for, and what action you need to take. You can write this down in your asthma action plan.
How much daily change is normal?
The scores you get, and any changes from them, are personal to you. You and your GP or asthma nurse can agree what changes you need to look out for and what action you need to take.
It is usual to see slight differences, either between morning and evening scores, or from one day to the next . Your GP or asthma nurse will be looking at how much lower your score is compared to your personal best score.
- If your score is 80% of your personal best score and you don’t have symptoms, this is usually normal and nothing to worry about.
- If your score is 50%-80% of your personal best score you should speak to your GP or asthma nurse.
- If your score is 50% or less than your personal best score you need to take urgent action or call 999.
Always use an asthma action plan
alongside your peak flow diary so you know what to do if asthma symptoms get worse.
Where can I get a peak flow meter?
You can get a peak flow meter on prescription from your GP or asthma nurse . If you pay for your prescriptions, you’ll need to pay the usual cost for one peak flow meter.
You can also buy a peak flow meter yourself, from a pharmacy or online. If you’re buying one for a child, it should have a smaller mouthpiece and a lower scale.
Most peak flow meters come with a peak flow calendar to note your scores. You can also download our peak flow diary.
Inhaler choices
Did you know that managing your lung condition well could help you feel your best and help the environment? We’ve partnered with the NHS to support you to make changes, so that you can live better with your lung condition and help the environment at the same time.
Find out more about inhaler choices.

Get support
Call our Helpline for support with your condition. Get advice on your medicines, symptoms or travelling with a lung condition, or just call us to say hello.




